Your second skin
A long-ignored body tissue could be a new sensory organ that holds the key to tackling chronic pain.
Caroline Williams investigates
SCIENTIFIC revelations come from the Unlikeliest of places. Like a rat, in a lab, doing a “downward dog” stretch. According to the people who found a way to get rats to do yoga, these creatures benefit from a good stretch as much as we do. In the process, they are revealing the true significance of a body tissue that has been overlooked by science for centuries.
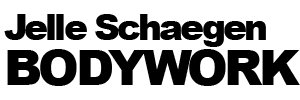
The 19th-century anatomist Erasmus Wilson called this tissue—now known as fascia—a natural bandage. In dissection, that is exactly what it looks like: sheets of white, fibrous connective tissue that are strong yet flexible and perfect for keeping muscles and organs in place. They are also sticky, gloopy and get in the way of looking at the muscles, bones and organs they cover. Which explains why, for years, anatomists cut this tissue off, chucked It away and thought little more about it.
Recently, though, researchers have begun to take a fresh look at fascia and are finding that it is anything but an inert wrapping. Instead, it is the site of biological activity that explains some of the links between lifestyle and health. It may even be a new type of sensory organ. than is commonly appreciated,” says Karl Lewis at Cornell University in Ithaca, New York.
We are now realizing that a better understanding of this ubiquitous tissue is sorely needed. If we manage to figure it out, it has the potential to provide “There appears to be more going on in the fascia
new ways to tackle many common yet hard-to-treat conditions, from immune dysfunction to chronic pain.
One difficulty with studying fascia is that there is disagreement about what it actually is. It comes under the umbrella of connective tissue, which, at its broadest definition includes not only tendons and ligaments, but also bone, skin and fat.
Most fascia researchers, however, understand it to be sheets of tissue made up of strong collagen fibres and stretchy elastin fibres. In many places, these fibrous sheets are separated by “areolar” or “loose” fascia, a form that contains fewer fibres and with the gaps between fibres filled with a slimy substance that allows the surrounding layers to slide over each other. The main ingredients of this slippery soup are hyaluronic acid, for lubrication, and proteoglycans, molecules that provide cushioning. The fascia fibres and the soup are both secreted by specialized calls in the tissue- fibroblasts and the recently discovered fasciacytes.
Holding us together
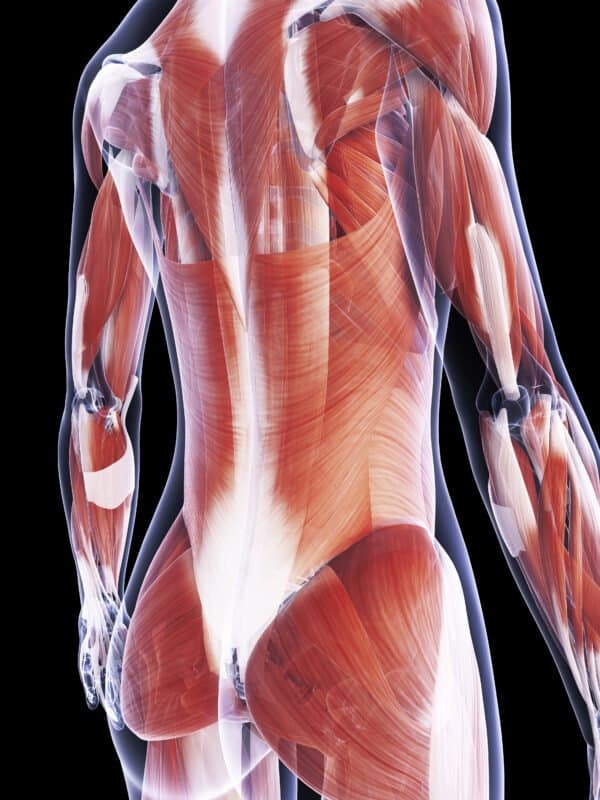
If you were to cut into the body, you would find two obvious layers of this natural cling film: the superficial fascia, which sits directly under the skin, and the deep fascia, which wraps muscles and organs and connects them to each other.
Some researchers, however, extend the definition to include the visceral fascia, which lines the body cavity and divides it into compartments for different organs, and also thin layers of connective tissue that line pretty much every part of the body. By this definition, fascia forms a network that pretty much holds us together.
Remarkably, until the early 2000s, no one had studied this common tissue in detail.
Among the first to do so was Carla Stecco, an orthopaedic surgeon and anatomist at the University of Padova in Italy. She started studying fascia 20 years ago when her father, a physiotherapist called Luigi Stecco, invented a form of physical therapy called fascial manipulation, which he claimed could treat everything from headaches to muscle and joint pain. His system is now one of many physical therapies that hinge on the idea that fascia can become stiff, and that it can be “released” through massage.
The only problem was that there was no evidence for or against the idea that physically manipulating the body did anything specifically to the fascia, or that this would affect pain. And as Carla Stecco soon discovered, there wasn’t even a body of literature explaining, in detail, what fascia actually was. It wasn’t even known if it had nerves associated with it, she says. Since then, she and others have shown that fascia is indeed rich in nerves, and that the information that these relay varies throughout the body. Superficial fascia contains nerves that specialize in sensing pressure, temperature and movement.

Deep fascia is involved in proprioception, the body’s sense of its position in space, and nociception, the sensing of pain. Because of this sensory role, some researchers say that fascia should be considered a new organ, one that is Specialized for communication about the body’s internal state. Robert Schleip at the Technical University of Munich in Germany recently estimated that an adult’s fascia contains approximately 250 million nerve endings, similar to, or slightly more than the skin. “It is beyond any doubt our richest sensory organ,” he says.
Others are more cautious. “It’s plausible, but there is a strict definition for an organ to do with material organization, cell types and function, so it sounds like it’s a candidate,” says Lewis. “But it’s early days for making that determination.” Organ or not, there is evidence that deep fascia specializes in a different kind of message to other bodily tissues.
Experiments in which healthy human volunteers had painful injections into their skin, muscles and fascia showed that while nerves in the skin and muscles produce focused, localized pain, the network of nerves in fascia is linked to a radiating pain, one that is more difficult to pinpoint. This kind of diffuse pain is a feature of several chronic pain disorders, including fibromyalgia, which some studies have linked to inflammation in the fascia. It is also a feature of post-exercise soreness, which has long been blamed on damage to the muscles, but which some researchers now think has more to do with injury or inflammation in the fascia.
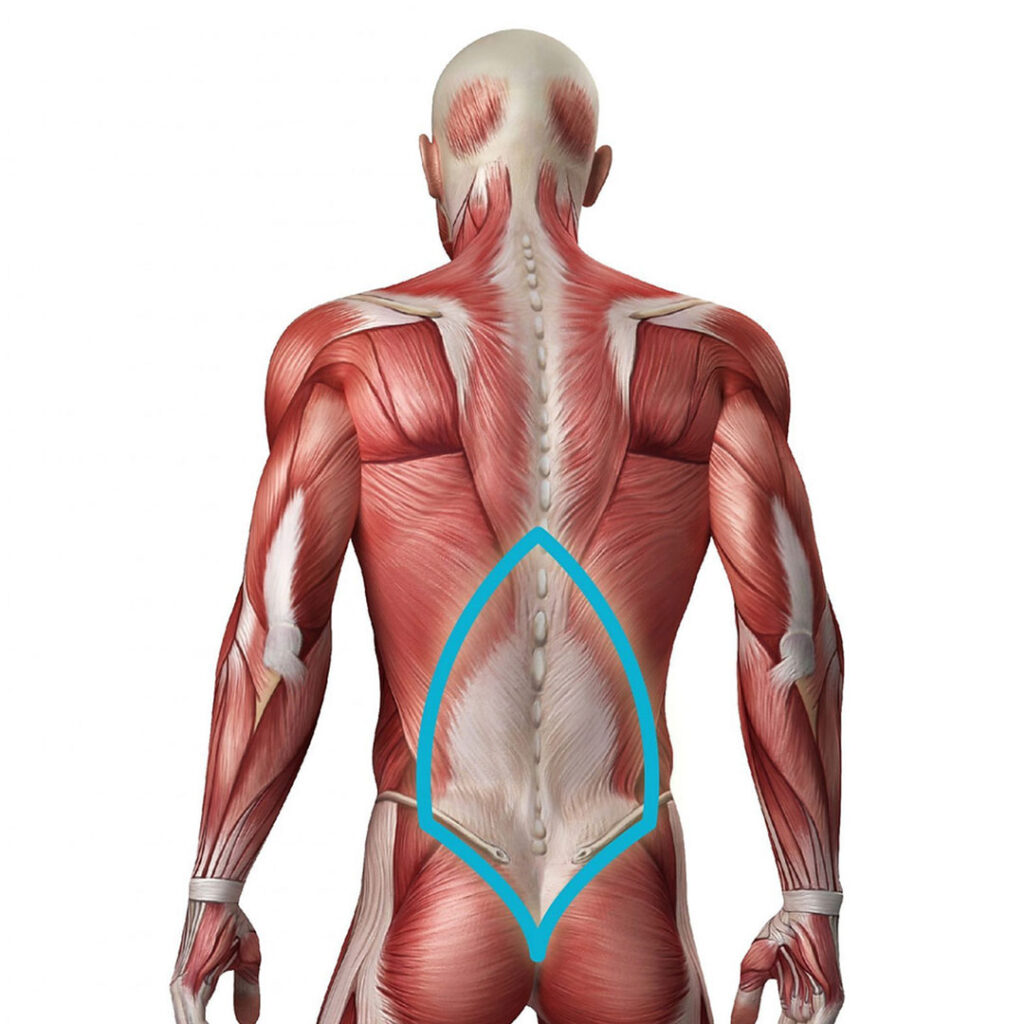
The bad news for anyone with inflamed fascia is that if it continues for too long, the body responds by altering the composition of fascial nerves to become more sensitive to pain. In rats, the percentage of nociceptive fibres —pain receptors that respond to harmful stimuli—in the fascia increased from 4 per cent to 15 per cent following chronic inflammation of deep fascia in the lower back.
This could help to explain why lower back pain is so difficult to treat. Despite being one of the most common causes of work absence and overall movement restriction, 85 per cent of cases worldwide are classified as non-specific, meaning the exact cause can’t be established.
Given what we now know about nerves in the fascia, the thoracolumbar fascia, a diamond-shaped, multi layered structure in the lower back in which different layers connect to different muscle groups in the trunk, is starting to look like a good place to put the blame for this back pain. “The thoracolumbar fascia is like a big receptor that is able to feel the tension coming from the upper limbs, the spine and the abdomen,’ says Stecco. The sensory neurons in the fascia may respond to this tension by registering it as pain.
On top of nerve changes, inflammation in the loose, areolar fascia that is found between fascial layers can make matters worse. Helene Langevin at the US National Institutes of Health in Maryland used ultrasound imaging of the lower back to show that people with chronic lower back pain had thoracolumbar fascia that was 20 per cent stiffer than those without this pain.
This stiffness seemed to be explained by multiple layers of tissue becoming stuck together, stopping the loose layer from sliding. Her studies in pigs have backed this up, showing that even after an initial injury has healed, a lack of movement in the lower back can be enough to keep the fascia stiff and to cause adhesions, where two layers become physically linked by new collagen fibres. This, other studies suggest, restricts movement, not only in the fascia immediately surrounding.
A body-wide network
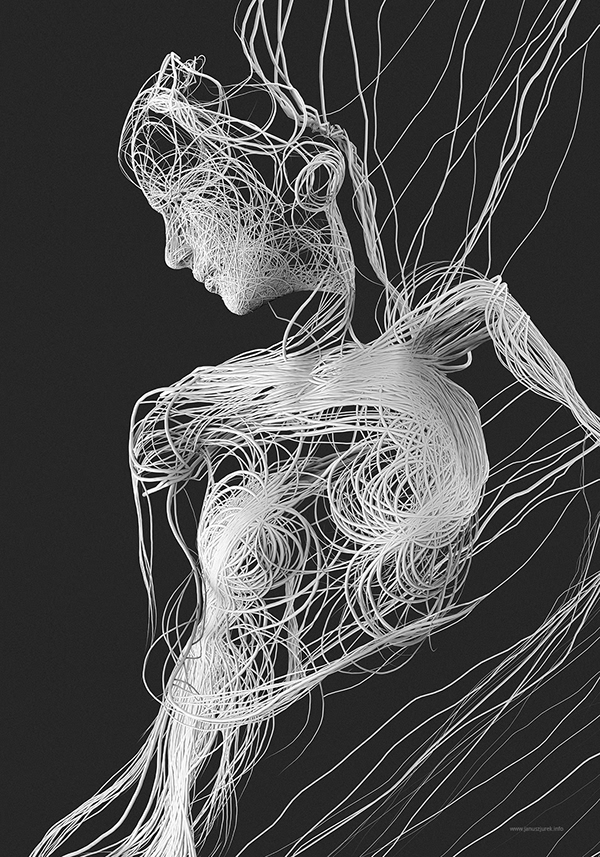
Our understanding of how fascia affects health (see main story) depends on where you draw the line between where it begins and ends in the body. Some people think that as well as the distinct layers of this tissue found under the skin and surrounding muscles, the term should also cover the interstitium: the fluid-filled connective tissue that lines every organ, muscle fibre and blood vessel. If that is correct, the fascia makes a whole-body network of fluid that could function both as a shock absorber and an immune network relevant to inflammatory disorders, scar formation and the spread of cancer. The true nature of the interstitium only became apparent in 2018 when a study by Neil Thiese at the Icahn School of Medicine at Mount Sinai, New York, and his colleagues used a new microscopic technique to look at its structure in a living person undergoing a biopsy.
In the past, it was only possible to see this tissue by removing it and squashing it on a microscope slide. When seen in living tissue, what had previously looked like a dense tangle of fibres actually had a sponge-like structure filled with fluid that drained into the lymphatic system, part of the body’s immune set-up.
The team suggested that physical movement may help keep this fluid healthy, whether due to the pumping of the heart, the movement of the digestive tract or physical movement of the body. “It seems that no such spaces are static,” says Thiese. This discovery opens up the possibility that the body is connected in ways that we are only beginning to understand and that movement is required to keep this tissue healthy.
The stiff spot, but also in connected regions nearby. In particularly severe cases, fascial layers can become stuck into one immobile block that runs from the superficial fascia to the deep fascia and into the muscle.
Injury and inflammation aside, there are many other reasons why fascia may become stiff, Schleip’s research hints that activation of the sympathetic nervous system, which is involved in the body’s fight-or-flight response, causes the fascia to contract by prompting the fibroblasts within it to transform into myofibroblasts, cells that are part of the inflammatory response to injury, often seen in joint-related problems such as frozen shoulder. The details of how exactly fight-or-flight stress leads to stiffness are still being worked out, but Schleip says that adrenaline seems to increase the expression of an inflammatory substance called TGF-beta. This is then stored in the loose fascia in preparation for the next time the body is stressed. When this happens, fibroblasts “drink [TGF-beta] and they become myofibroblasts in a few hours”, he says. ‘And then they are four times as strong as before.
They are contraction machines. So, adrenaline can make fascia stiffer.” in fact, the list of things that affect fascial stiffness is getting longer all the time. “Oestrogen is able to create a fascia that is more elastic” says Stecco. “The fascia is a very dynamic tissue that is able to answer to hormonal input, chemical input and mechanical input. Altogether, that defines if our fascia is elastic or rigid.” On the plus side, this dynamic nature of fascia suggests that lifestyle changes could help to reverse problems related to it. One promising intervention under investigation is stretching. In samples of rat tissue, Langevin found that stretching causes changes to the fibroblasts that make up the matrix of the loose fascia. She says they expand several fold and become longer and flatter. “Stretching the tissue allows it to relax,” she adds.
Stretch it out
Other studies by Langevin with pigs showed that stretching the lower back for 5 minutes, twice a day, not only reduced the size of an area of inflammation, but also seemed to Induce a series of anti-inflammatory chemical events from the fascia. This is a promising finding because chronic inflammation has been linked to pretty much every modern ailment going, from heart disease and diabetes to cancer and depression.
A team at Harvard Medical School is conducting a trial in people to find out if the same is true in humans. A pilot study completed in late 2021 showed that healthy volunteers who undertook an hour-long stretching session had altered levels of immune system molecules called cytokines, compared with those who didn’t stretch, suggesting that there is a regulation of inflammation after stretching. Future studies will assess whether levels of resolvins, chemicals made by the body that turn off inflammation, also increased, as has been seen in rat and pig stretching studies. If so, stretching could prove useful for reducing cases of more widespread chronic inflammation, which can be triggered by long-term stress, obesity and bad diet.
As for physical therapies that focus on fascia release, such as massage, itis unclear whether they have the same cellular and anti-inflammatory effects as stretching seems to, or whether they simply make temporary changes to the fascia. It could be, for example, that manual therapies warm the tissues, which has been shown to make the fascia matrix less viscous, temporarily allowing the layers to slide more easily. Langevin sounds a note of caution, that until more is known about what happens during these therapies, it isn’t clear what, if anything, they do to the fascia, or anything else.
In order to turn fascia research into evidence-based treatments, this tissue will also have to overcome its image problem among scientists. This dates back to the1940s and 50s, when medical researchers were paying little attention to the stuff, and it became central to an alternative approach to health invented by the late biochemist Ida Rolf. Her method, which she called structural integration, but which is better known as Rolfing, is a mixture of physical therapy and claims about alignment of bodily energy fields. Since then, fascia has become a buzz word in all kinds of alternative therapies.
Stecco, however, thinks that itis high time for the mainstream medical profession to start paying attention to this tissue. She would like fascia to be recognized as important to many areas of medicine, and as a window into our overall health. This, she says, would be “the true revolution of the fascia”.
Caroline Williams is a freelance writer based in Godalming, Surrey,
UK, and author of Move! The new science of body over mind